Healthcare data security is not just an IT concern, but a fundamental pillar of patient care and organizational survival. From electronic health records (EHRs) to connected medical devices and cloud-based systems, the sector has embraced innovation. But with that innovation comes risk.
According to Sophos, 67% of healthcare organizations experienced ransomware attacks in 2024. And another study shows that healthcare has long been a big target: from 2005 – 2019, over 249 million individuals’ health records were exposed, with the number and severity of breaches increasing over time.
What is Healthcare Data Security?
Healthcare data security encompasses the strategies, technologies, and policies designed to protect sensitive patient information from unauthorized access, alteration, or destruction. The shift from paper-based records to digital systems has amplified risks, making robust security frameworks essential to prevent identity theft, insurance fraud, and clinical disruptions
The healthcare industry holds some of the most sensitive data imaginable: not just names and Social Security numbers, but detailed medical histories, diagnoses, prescriptions, and insurance information. This makes it an especially attractive target for cybercriminals, who can monetize data or weaponize access.
But beyond financial damage (which averages $10.93 million USD per breach), breaches carry profound human consequences. Ransomware attacks, for instance, can paralyze hospital operations, delaying treatments and endangering lives.
Healthcare data security is about more than compliance—it’s about protecting lives.
The Regulatory Environment: High Stakes, Complex Requirements
In the United States, HIPAA remains the backbone of healthcare data regulation, mandating specific safeguards to protect electronically protected health information (ePHI). The HIPAA Security Rule divides these requirements into three categories: administrative (like workforce training and risk assessments), physical (like secure facility access), and technical (like encryption and audit trails).
But HIPAA isn’t the only standard. Many healthcare providers must also navigate the General Data Protection Regulation (GDPR) when serving EU residents, and increasingly, new state-level laws such as the California Consumer Privacy Act (CCPA).
Penalties for noncompliance can be staggering. HIPAA violations can carry fines of up to $1.5 million per year, and in some cases, criminal prosecution.
A Threat Landscape That’s Rapidly Evolving
Cyber threats targeting healthcare are becoming more advanced and more frequent. Ransomware remains one of the most disruptive attack vectors, encrypting mission-critical systems and demanding payment for access. Attackers often gain entry via phishing emails that appear to come from trusted internal sources, making them dangerously effective.
Meanwhile, distributed denial-of-service (DDoS) attacks have surged, knocking out trauma centers and delaying care. Insider threats—both intentional and accidental—continue to account for a significant share of breaches. And with Internet of Medical Things (IoMT) devices now part of daily operations, the attack surface has grown exponentially. Devices such as insulin pumps, infusion machines, and CT scanners can all be manipulated to compromise care.
One particularly troubling trend is the continued reliance on legacy systems. These outdated infrastructures often lack the security patches and architecture needed to defend against modern attacks.
Why Traditional Monitoring Isn’t Enough for Robust Healthcare Data Security
Historically, many healthcare organizations have relied on perimeter firewalls, antivirus software, and periodic audits to manage security. While these tools remain part of a robust defense-in-depth strategy, they’re not sufficient on their own.
The growing complexity of hybrid environments—spanning on-premises servers, cloud platforms, and edge devices—requires a more sophisticated approach.
Improving Healthcare Data Security with Network Observability
Network observability goes beyond traditional monitoring by offering deep visibility into every layer of your infrastructure. From system-level performance metrics to real-time threat detection, it enables a proactive security posture that evolves with the threat landscape.
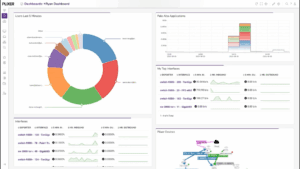
A network observability & defense platform like Plixer One can analyze patterns in real-time across complex ecosystems, including cloud applications, EHR databases, and IoMT devices. This enables IT teams to flag unusual behaviors such as:
- Sudden spikes in encrypted traffic
- An unauthorized device accessing patient records at odd hours
- Lateral movement of data across subnetworks that are normally isolated
These anomalies are often the first indicators of an unfolding cyberattack. Plixer One’s ability to correlate telemetry from a wide variety of different sources allows for rapid identification and containment.
Accelerating Incident Response with Contextual Intelligence
When a breach does occur, response time is everything. Network observability shortens this window by equipping teams with the context needed to act decisively. Rather than sifting through fragmented logs after the fact, platforms like Plixer One provide:
- Detailed timelines of attack vectors
- Visual mapping of compromised systems
- AI-driven context and actionable data
This accelerates root cause analysis and helps prevent further escalation.
Defending IoMT and Legacy Systems
One of the most pressing challenges in healthcare security is managing legacy systems and connected medical devices, many of which were never designed with cybersecurity in mind. Plixer One can profile device behavior and baseline normal operations. When something deviates—like a CT scanner transmitting data to an unauthorized IP address—it’s flagged instantly.
Mitigating Third-Party and Supply Chain Risk
With more than half of breaches linked to third-party vendors, observability is essential for protecting the supply chain. Whether it’s an external billing service or a cloud-based imaging solution, observability platforms can track:
- API call volumes and destinations
- Data access frequency and scope
- Anomalies in cloud usage behavior
This visibility helps ensure that partners don’t introduce vulnerabilities into your environment.
Looking Ahead: Predictive Defense Through AI and ML
Forward-thinking observability platforms integrate artificial intelligence and machine learning to go beyond detection and into prediction. By continuously learning from historical behavior, these platforms can forecast which systems are most likely to be targeted and suggest preemptive hardening actions.
Concluding Thoughts
Healthcare data security requires a proactive, layered approach—and network observability is a critical enabler.
Platforms like Plixer One give organizations the visibility, intelligence, and automation needed to respond to threats in real time, protect legacy systems, and build a future-ready security posture.
To see how Plixer One can help secure your unique environment, book a personalized demo with one of our engineers today.