It starts with a twinge. Then a limp. By the time our patient reaches the orthopedic surgeon, they’re facing full knee replacement surgery—a journey that will take them through pre-op assessments, the OR, recovery, and months of rehabilitation.
But here’s what most patients don’t see: behind every successful outcome is a network that facilitated excellent patient care, from ensuring staff always has accurate information at their fingertips, to keeping patient data safe despite healthcare being a large target for cyberattacks.
For NetOps and SecOps teams in healthcare, this patient journey is a stress test of every system, connection, and security protocol you’ve built. And when something goes wrong with your network, the consequences ripple through every aspect of care.
The Anatomy of a Healthcare Network Crisis
Pre-op day, 6:47 AM. The radiologist can’t access the latest imaging. The delay ripples from the OR schedule to discharge planning. Meanwhile, IT is already underwater, juggling cloud-first applications, sprawling endpoints, and remote care connections that were never designed to work together.
Sound familiar? You’ve done the best you can with fragmented monitoring tools, but healthcare networks face unique challenges that traditional IT environments simply don’t encounter.
The Scale Challenge
Healthcare networks aren’t just big—they’re vast and diverse ecosystems that demand specialized attention. A typical hospital network might include:
- Legacy medical devices running on proprietary protocols that can’t be easily updated
- High-bandwidth imaging systems transferring massive DICOM files between departments
- Electronic Health Records (EHRs) handling thousands of concurrent users across multiple facilities
- IoT medical devices from infusion pumps to patient monitors, each with unique connectivity requirements
- Telehealth platforms supporting remote consultations and home monitoring
- Mobile devices used by staff, patients, and visitors throughout the facility
Each of these systems generates different types of network traffic, has different performance requirements, and presents unique security challenges. Traditional network monitoring tools that might work well in corporate environments often struggle with this heterogeneous mix because they weren’t designed to handle the specialized protocols and traffic patterns that medical devices generate.
The Uptime Imperative
In most IT environments, planned maintenance windows and brief outages are manageable inconveniences. In a worst-case healthcare scenario, they can be life-threatening. Consider these situations:
During Surgery: An anesthesiologist needs real-time access to patient vitals, medication histories, and lab results. Network latency of even a few seconds can impact critical decisions about anesthesia levels or emergency interventions.
Emergency Department: Trauma patients arrive with incomplete medical histories, and staff need immediate access to regional health information exchanges, insurance systems, and specialist consultation platforms. A network delay during a cardiac arrest can mean the difference between life and death.
Intensive Care Units: Continuous monitoring devices generate streams of data that must be processed, stored, and made available to care teams instantly. Any interruption in data flow could mean missing a critical change in patient condition—a dropped heartbeat, a dangerous medication interaction, or a ventilator malfunction.
The Compliance Maze
On top of everything else, healthcare networks must also navigate regulatory requirements that go far beyond typical IT compliance frameworks:
HIPAA Compliance demands that every packet carrying patient data be encrypted, logged, and protected according to strict federal guidelines. This includes not just obvious PHI like names and addresses, but also metadata that could be used to identify patients.
HITECH Act Requirements mean that any security incident must be thoroughly investigated and documented. Network visibility tools must provide the forensic capabilities to prove what data was accessed and by whom—a requirement that can make or break regulatory audits.
State and Local Regulations add additional layers of complexity, with many states having specific privacy requirements that affect how patient data can be transmitted and stored across networks.
The challenge isn’t just meeting these requirements, but doing so while maintaining the performance and availability that patient care demands.
What Healthcare Teaches Us About Network Visibility
Lesson 1: Prevention Beats Reaction
In healthcare, the best treatment is often prevention. A cardiologist doesn’t wait for a heart attack to recommend lifestyle changes—they monitor risk factors and intervene early. The same principle applies to network management, but the stakes in healthcare networking make this lesson even more critical.
Traditional reactive approaches wait for users to report problems, then scramble to identify root causes while systems remain degraded. In healthcare, this might mean:
- Surgical delays while radiology systems are restored
- Medication errors due to inaccessible patient records
- Staff using dangerous workarounds that bypass security controls
A proactive visibility approach transforms this dynamic entirely. Continuous monitoring of network flows, performance metrics, and security indicators allows teams to identify and resolve issues before they impact patient care. This includes anomaly detection that spots unusual traffic patterns before they become outages, predictive analytics that identify devices likely to fail, and automated remediation that can isolate problematic network segments without human intervention.
The difference becomes most apparent during critical moments. Instead of discovering that the PACS system is down when a radiologist tries to access imaging during an emergency, proactive monitoring would have detected the performance degradation hours earlier, allowing IT to address the issue during a less critical time.
Lesson 2: Context Is Everything
A skilled diagnostician doesn’t just look at symptoms—they understand the patient’s full history, current medications, and how different systems interact. They know that chest pain in a 25-year-old athlete requires different investigation than the same symptom in a 65-year-old diabetic.
Your network monitoring should work the same way. When the physical therapist can’t access patient vitals during recovery, an issue with the EHR application isn’t the only possible cause, or even the most likely one. The issue might be:
Bandwidth Saturation: A forgotten backup process consuming network resources during peak hours, or a new medical device that wasn’t properly configured for QoS prioritization.
Security Policy Conflicts: Firewall rules updated for one system that inadvertently blocked traffic for another, or certificate renewals that weren’t coordinated across integrated systems.
Infrastructure Interdependencies: A seemingly minor switch failure creating a cascade of connectivity issues across multiple departments, or DNS resolution problems that only affect certain types of medical devices.
Application Performance Issues: Database queries that have degraded over time due to data growth, or API calls between systems that are timing out due to increased load.
End-to-end visibility means understanding not just what’s happening, but why it’s happening and how it affects the entire care pathway. This requires a solution like an observability platform that can correlate data across multiple layers of the infrastructure stack, providing the contextual information needed to distinguish between symptoms and root causes.
Lesson 3: Every System Must Work Together
Healthcare is fundamentally about connected care. The patient portal must seamlessly integrate with the EHR. Imaging systems need to share data with both radiology workstations and referring physicians. Telehealth platforms must access the same patient records as in-person visits. Mobile applications used by home health nurses must sync with hospital systems in real-time.
This level of integration creates complex dependencies that traditional monitoring tools struggle to map and manage:
East-West Traffic: Most healthcare network traffic flows between systems within the organization rather than to external destinations. Traditional perimeter-focused monitoring misses these internal communications that are critical to patient care.
API Dependencies: Modern healthcare applications rely heavily on API calls between systems. A single patient lookup might trigger dozens of API calls to different services, each with its own performance characteristics and failure modes.
Data Synchronization: Patient data must remain consistent across multiple systems, often with different update frequencies and synchronization mechanisms. Network delays or failures can create dangerous inconsistencies where information is up-to-date on one system and outdated on another.
Hybrid Cloud Complexity: Many healthcare organizations operate environments that span on-premises legacy systems, cloud-based applications, and SaaS platforms. Each environment has different monitoring requirements and visibility challenges.
Your network is the connective tissue that makes integrated care possible. But fragmented monitoring tools create blind spots that leave you guessing about performance issues, security threats, and compliance gaps.
The Cost of Network Blindness
The real cost of network issues in healthcare isn’t just measured in IT tickets or system performance, but in delayed procedures, frustrated staff, and compromised patient safety.
When Imaging Systems Fail
PACS (Picture Archiving and Communication System) network issues create ripple effects that extend far beyond the radiology department:
- Diagnostic delays as physicians can’t access current or historical images
- Surgical postponements when pre-operative imaging isn’t available
- Duplicate procedures when staff can’t confirm whether tests have already been performed
- Compliance violations if images aren’t properly stored or transmitted according to retention policies
EHR Access Interruptions
Electronic Health Record systems are the backbone of modern healthcare, and network issues that affect EHR access create immediate patient safety risks.
Medication errors can occur when staff can’t access current prescription lists or allergy information, potentially leading to dangerous drug interactions. Duplicated treatments happen when providers can’t see what has already been done, wasting resources and potentially harming patients. Incomplete documentation affects both patient care and legal compliance, creating gaps in the medical record that can have long-term consequences.
Perhaps most concerning, staff frustration with unreliable systems can lead to workarounds that bypass security controls, creating additional vulnerabilities in an already complex security landscape.
Security Incidents and Their Ripple Effects
Network visibility gaps that allow security threats to go undetected create risks that extend beyond typical IT concerns:
- Ransomware attacks that can shut down entire hospital systems
- Data breaches that expose sensitive patient information
- Regulatory penalties that can reach millions of dollars
- Reputation damage that affects patient trust and organizational credibility
Each of these scenarios represents a failure of network visibility. You can’t fix what you can’t see, and you can’t prevent what you don’t understand.
Building a Proactive Approach
That knee replacement patient needs a seamless care experience, and total, proactive visibility into your network is key. This means moving beyond traditional monitoring approaches to embrace comprehensive network observability.
Unified Monitoring Across All Environments
Healthcare networks are inherently hybrid, spanning multiple locations, cloud providers, and technology stacks. Complete visibility comprises:
On-Premises Infrastructure: Deep packet inspection and flow analysis for legacy medical devices and core hospital systems that can’t be moved to the cloud. This includes specialized monitoring for medical device protocols that don’t conform to standard IT networking patterns.
Cloud Applications: Native cloud monitoring that understands the unique performance characteristics of SaaS EHR systems, cloud-based imaging platforms, and telehealth services. This requires tools that can monitor application performance, not just network connectivity.
Mobile and Remote Access: Visibility into the network experience of mobile devices, home health workers, and patients accessing portals from various locations. This includes understanding how network performance affects the user experience across different devices and connection types.
IoT Medical Devices: Specialized monitoring for the growing ecosystem of connected medical devices, each with unique protocols and security requirements that demand tailored visibility approaches.
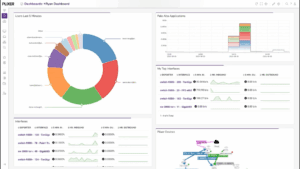
Real-Time Intelligence for Proactive Management
Flow data analytics enable you to continuously analyze network traffic patterns to identify anomalies, security threats, and performance degradations before they affect patient care. AI/ML-driven insights can automate the detection of unusual patterns that might indicate device failures, security breaches, or performance issues. Predictive analytics help IT teams prepare for capacity needs, planned maintenance, and system upgrades before problems occur.
Most importantly, contextual alerting provides not just notifications of what is happening, but insights into why it’s happening and what actions should be taken. This transforms alerts from interruptions into actionable intelligence.
Proactive Security for Patient Data Protection
Healthcare organizations face unique security challenges that require specialized network visibility:
Threat Detection: Real-time identification of malware, ransomware, and data exfiltration attempts that specifically target healthcare networks and understand the unique attack vectors that threat actors use against medical devices.
Compliance Monitoring: Automated tracking of data flows to ensure HIPAA compliance and support audit requirements, with the ability to prove that patient data is being handled appropriately across all network segments.
Incident Response: Forensic capabilities that can quickly determine the scope and impact of security incidents, providing the detailed evidence needed for breach notifications and regulatory reporting.
Zero Trust Architecture: Network visibility that supports microsegmentation and least-privilege access models while maintaining the performance required for patient care.
The Path Forward: From Reactive to Proactive
Our knee replacement patient is walking again. Their records, care plans, and appointments flowed smoothly across systems because IT made it happen behind the scenes.
But this success story represents more than just good IT support—it demonstrates the transformative power of proactive network management. Instead of waiting for problems to occur and then scrambling to fix them, healthcare IT teams can prevent issues before they impact patient care.
But moving from reactive to proactive network management requires a strategic approach:
Start with Critical Pathways: Identify the network communications that are most critical to patient care and ensure comprehensive monitoring of these paths first. This might mean prioritizing visibility into connections between the EHR and pharmacy systems or ensuring complete monitoring of the network paths that support critical care monitoring devices.
Integrate with Existing Systems: Network visibility tools should complement existing IT infrastructure rather than requiring wholesale replacement. Choose solutions that can work with existing network hardware, integrate with current security tools, and provide data that enhances rather than duplicates existing monitoring capabilities.
Train for Success: Staff need training not just on new tools, but on proactive thinking and incident prevention strategies. This includes understanding how to interpret predictive analytics, how to respond to early warning indicators, and how to use network visibility data to support capacity planning and system optimization.
Measure Impact: Track metrics that matter to healthcare outcomes, not just traditional IT performance indicators. This includes measuring improvements in system availability during critical procedures, reductions in security incidents, and improvements in compliance audit results.
Concluding Thoughts
Healthcare organizations that invest in comprehensive network visibility gain significant advantages that extend beyond IT operations. Improved patient outcomes result from faster, more reliable access to patient data that enables better clinical decision-making. Enhanced staff satisfaction comes from eliminating frustrating technology issues that allow healthcare workers to focus on patient care. Reduced operational costs follow naturally from preventing problems rather than fixing them after they occur.
Your network visibility strategy shouldn’t leave you fighting fires—it should give you the tools to prevent them.
Want to see a real-world use case? Read how Capstone Rural Health used Plixer One’s observability & defense capabilities to help deliver world-class patient care.